Cardiac arrest remains a critical medical emergency where every second counts. The introduction of ultrasound in cardiac arrest management has opened new diagnostic and therapeutic perspectives. However, its use must not compromise the quality of cardiopulmonary resuscitation (CPR). The CASA (Cardiac Arrest Sonographic Assessment) protocol has been developed to integrate ultrasound effectively and safely into cardiac arrest management. This article focuses on the practical implementation of CASA, particularly emphasizing the need to limit CPR interruptions to a maximum of 10 seconds during ultrasound assessment.
The CASA Protocol: Fundamental Principles
CASA is a targeted ultrasound protocol designed to be performed quickly during rhythm and pulse check pauses in CPR. Its main objective is to identify reversible causes of cardiac arrest without prolonging CPR interruptions.
Key Objectives of CASA:
-
- Rapidly identify reversible causes of cardiac arrest
- Guide therapeutic interventions
- Evaluate CPR effectiveness
- Aid in decision-making regarding continuation or termination of resuscitation efforts
The Golden Rule: 10 Seconds Maximum
The cornerstone of the CASA protocol is the strict limitation of ultrasound assessment to a maximum of 10 seconds. This rule is crucial for several reasons:
-
-
- **Maintaining cerebral and coronary perfusion**: Studies have shown that beyond 10 seconds of interruption, cerebral and coronary perfusion drops significantly, compromising the patient’s chances of survival [1].
-
-
-
- **Compliance with international recommendations**: American Heart Association (AHA) guidelines recommend limiting CPR interruptions to less than 10 seconds [2,3].
-
-
-
- **Optimization of chest compression fraction**: A high chest compression fraction (the time during which compressions are effectively performed) is associated with better survival outcomes [4].
-
Practical Implementation of CASA in 10 Seconds
To perform CASA effectively in 10 seconds, a systematic approach and meticulous preparation are essential.
-
-
-
Preparation before CPR Interruption
-
-
– Position the ultrasound machine next to the patient
– Select the appropriate probe (usually the cardiac probe)
– Adjust device settings (depth, gain) before interruption
– Brief the team on timing and roles
-
-
-
CASA Execution
-
-
– Clearly announce “Pause for ultrasound in 3, 2, 1”
– Quickly place the probe in the subxiphoid position during CPR
– Start recording the echography during CPR
– Stop chest compressions
– Obtain a view of the heart in less than 5 seconds
– Reposition the probe to get a clear view
– Announce “Resume compressions in 3, 2, 1”
– Wipe the chest with a towel
– Immediately resume CPR
-
-
-
Interpretation and Communication
-
-
– While CPR resumes, the operator analyze the recording and quickly communicates observations to the team
– Therapeutic decisions are made without interrupting CPR again
Techniques to Optimize CASA in 10 Seconds
-
-
- **Use of the subxiphoid view**: This view is generally the quickest to obtain and can be performed without interfering with cardiac massage [5].
-
-
-
- **Pre-positioning of the probe**: Place the probe on the patient just before CPR interruption to save time.
-
-
-
- **Use of a dedicated timer**: Designate a team member to strictly time the 10 seconds and count out loud.
-
-
-
- **Image recording**: Use the video clip function to record images during the 10 seconds, allowing for more detailed analysis after CPR resumption.
-
-
-
- **Clear and concise communication**: Use standardized terms to quickly communicate results to the team.
-
Sequential Assessment in CASA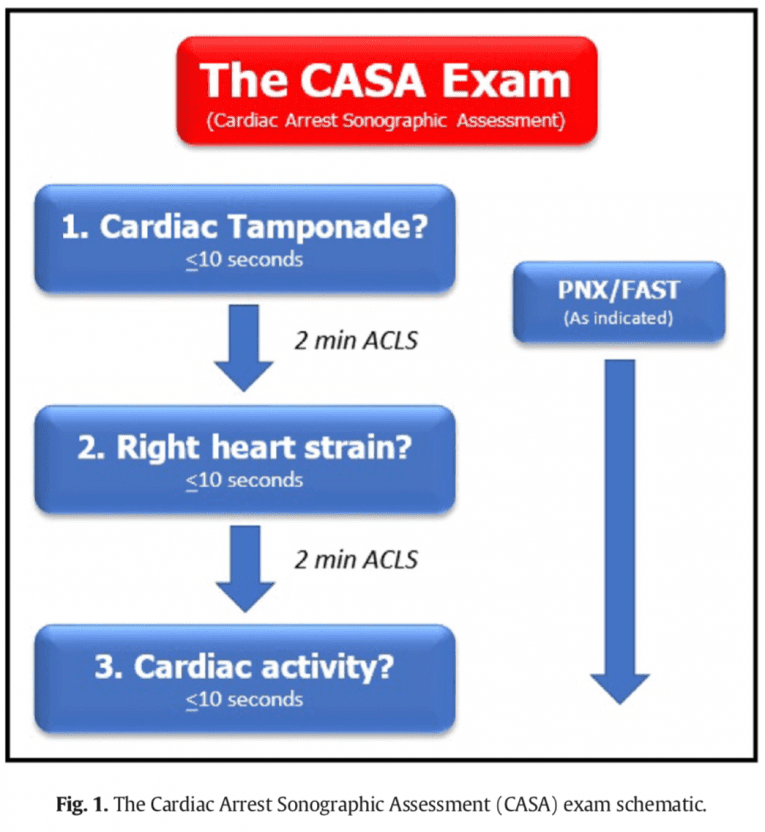
CASA proposes a sequential approach to evaluate different aspects without prolonging CPR interruption:
-
-
- **First cycle (0-10 seconds)**: Subxiphoid view to look for pericardial effusion.
-
-
-
- **Second cycle (if necessary, 0-10 seconds)**: Parasternal long axis view to evaluate ventricular function and look for right ventricular dilation.
-
-
-
- **Third cycle (if necessary, 0-10 seconds)**: Assess for cardiac activity
-
-
-
- **Fourth cycle (if necessary, 0-10 seconds)**: Rapid pulmonary assessment to look for pneumothorax.
-
The emphasis is on performing a single assessment per CPR cycle, prioritizing the most critical information.
Comparison with Other Ultrasound Protocols in Cardiac Arrest
Several ultrasound protocols have been developed for the evaluation of patients in cardiac arrest. Here’s a comparison of CASA with other commonly used protocols:
-
-
-
FEEL (Focused Echocardiographic Evaluation in Life Support)
-
-
The FEEL protocol, developed by Breitkreutz et al. [5], primarily focuses on cardiac evaluation.
**Advantages of CASA over FEEL**:
– More comprehensive evaluation including lungs and IVC (inferior vena cava)
– Better structuring with clearly defined steps
-
-
-
CAUSE (Cardiac Arrest Ultra-Sound Exam)
-
-
The CAUSE protocol, proposed by Hernandez et al. [6], is similar to CASA but with some differences.
**Differences between CASA and CAUSE**:
– CAUSE includes an evaluation of the abdominal aorta, not present in CASA
– CASA places more emphasis on IVC evaluation
-
-
-
SHoC (Sonography in Hypotension and Cardiac Arrest)
-
-
The SHoC protocol, developed by Atkinson et al. [7], is more comprehensive but potentially takes longer to perform.
**Advantages of CASA over SHoC**:
– Faster to execute, which is crucial in the context of cardiac arrest
– Focuses on the most common reversible causes
Unlike these protocols, CASA emphasizes rapid execution and minimization of CPR interruptions. The following table summarizes the key differences:
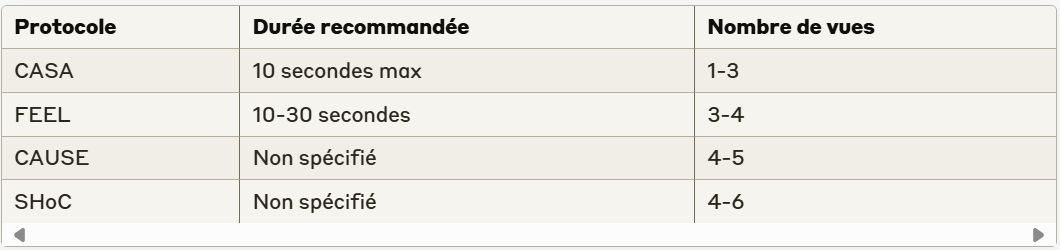
CASA distinguishes itself by its focus on strict limitation to 10 seconds, prioritizing CPR quality over the comprehensiveness of the ultrasound examination.
CASA Training
Training is crucial for effectively performing CASA in 10 seconds. It should include:
-
-
- **High-fidelity simulation**: Practice CASA in simulated cardiac arrest scenarios, with strict timing.
-
-
-
- **Repetitive drills**: Regularly train to quickly obtain key ultrasound views.
-
-
-
- **Teamwork**: Train the entire resuscitation team to integrate CASA without disrupting CPR.
-
-
-
- **Post-resuscitation debriefing**: Systematically analyze CASA performances after each real case.
-
Evidence on CASA Impact
Recent studies have shown the positive impact of CASA when performed respecting the 10-second limit:
– A study by Clattenburg et al. [8] showed that implementing a structured protocol like CASA could reduce the average duration of CPR interruptions for ultrasound from 21 to 10.1 seconds.
– Gaspari et al. [9] reported that the presence of cardiac activity on initial ultrasound (performed in less than 10 seconds) was associated with an odds ratio of 3.6 (95% CI: 2.2-5.9) for survival to hospital admission.
– A meta-analysis by Tsou et al. [10] showed that point-of-care ultrasound, when performed quickly, could identify reversible causes of cardiac arrest in 10 to 35% of cases, directly influencing management.
Challenges and Considerations
Despite its advantages, implementing CASA in 10 seconds presents challenges:
-
-
- **Learning curve**: Achieving the necessary competence to perform CASA in 10 seconds requires intensive practice.
-
-
-
- **Image quality**: Time constraint can sometimes compromise the quality of obtained images.
-
-
-
- **Distraction risk**: The team must stay focused on CPR and not be distracted by ultrasound.
-
-
-
- **Over-interpretation**: The risk of drawing hasty conclusions based on a very brief examination exists and must be recognized.
-
Conclusion
The CASA protocol represents a significant advance in integrating ultrasound into cardiac arrest management. By emphasizing strict limitation to 10 seconds of CPR interruption, it offers a balance between providing crucial diagnostic information and maintaining high-quality resuscitation.
Current evidence suggests that CASA, when properly implemented, can improve identification of reversible causes of cardiac arrest and potentially positively influence patient outcomes. However, its success relies on rigorous training, regular practice, and team discipline to maintain focus on high-quality CPR.
Challenges related to its implementation, particularly the learning curve and technical considerations, should not be underestimated. Nevertheless, with adequate training and careful integration into existing protocols, these obstacles can be overcome.
The future of CASA looks promising, with prospects for improvement thanks to technological advances such as artificial intelligence and automation. These developments could make CASA even faster, more accurate, and accessible, strengthening its role in optimizing cardiac arrest management.
References
[1] Kleinman ME, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S414-35.
[2] Link MS, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18 Suppl 2):S444-64.
[3] Soar J, et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100-47.
[4] Christenson J, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120(13):1241-7.
[5] Breitkreutz R, et al. Focused echocardiographic evaluation in life support and peri-resuscitation of emergency patients: a prospective trial. Resuscitation. 2010;81(11):1527-33.
[6] Hernandez C, et al. C.A.U.S.E.: Cardiac arrest ultra-sound exam—A better approach to managing patients in primary non-arrhythmogenic cardiac arrest. Resuscitation. 2008;76(2):198-206.
[7] Atkinson P, et al. International Federation for Emergency Medicine Consensus Statement: Sonography in hypotension and cardiac arrest (SHoC): An international consensus on the use of point of care ultrasound for undifferentiated hypotension and during cardiac arrest. CJEM. 2017;19(6):459-470.
[8] Clattenburg EJ, et al. Implementation of a Cardiac Arrest Sonographic Assessment protocol in a community emergency department. Am J Emerg Med. 2020;38(5):962-965.
[9] Gaspari R, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33-39.
[10] Tsou PY, et al. Accuracy of point-of-care focused echocardiography in predicting outcome of resuscitation in cardiac arrest patients: A systematic review and meta-analysis. Resuscitation. 2017;114:92-99.
