Here’s a reminder of the components of the Pediatric Assessment Triangle (PAT). For more information on the triangle, please refer to the article published on September 9, 2024, titled: The Pediatric Assessment Triangle: An Essential Tool in Emergency Care https://com-bos.ca/en/the-pediatric-assessment-triangle-an-essential-tool-in-emergency-care/
Components of the Pediatric Assessment Triangle
-
Appearance

Appearance is considered the most important side of the triangle, reflecting oxygenation, ventilation, cerebral perfusion, and central nervous system functioning.
Elements to evaluate:
– Tone: Is the child active, moving spontaneously, or floppy?
– Interactivity: Is the child alert, responsive to environmental stimuli?
– Consolability: Can the child be consoled or calmed?
– Gaze: Is the gaze lively and attentive or fixed and empty?
– Speech/cry: Are the cries strong and vigorous or weak and whimpering?
An altered appearance may indicate severe neurological, respiratory, circulatory, or metabolic impairment.
-
Work of Breathing
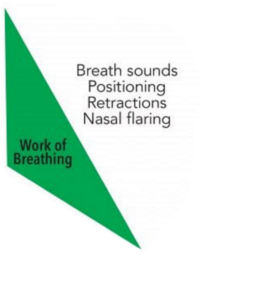
Assessing the work of breathing allows for quick identification of respiratory distress or impending respiratory failure.
Elements to evaluate:
– Abnormal position: Sitting position, tripod position, refusal to lie down
– Retractions: Supraclavicular, intercostal, subcostal
– Nasal flaring
– Audible breathing sounds: Stridor, wheezing, grunting
– Tachypnea or bradypnea
Increased work of breathing usually indicates respiratory pathology but can also be observed in other situations such as metabolic acidosis.
-
Circulation to the Skin
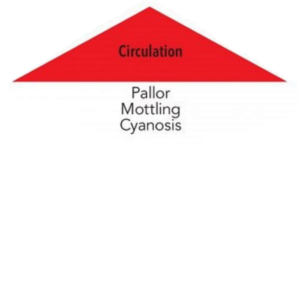
Assessing circulation to the skin allows for a quick appreciation of peripheral tissue perfusion.
Elements to evaluate:
– Color: Pallor, cyanosis, mottling
– Capillary refill time (CRT): Normally < 2 seconds
An alteration in skin circulation may indicate shock, severe dehydration, or circulatory insufficiency of another origin.
When an abnormality is detected in one of the components of the Pediatric Assessment Triangle, it is crucial to quickly initiate appropriate interventions. Here is a list of rapid interventions for each of the PAT components:
-
Interventions for Altered Appearance
An altered appearance may indicate a serious neurological, respiratory, circulatory, or metabolic problem. Immediate interventions may include:
– Securing the airway: positioning (place the baby so that the airways are clear, remove the baby from the car seat)
– Move the child to the intervention room and start continuous cardiorespiratory monitoring
-
Interventions for Altered Work of Breathing
An alteration in the work of breathing requires rapid action to prevent respiratory decompensation. Interventions may include:
– Optimal positioning: sitting or semi-sitting position, lying down with shoulders slightly raised
– Airway clearance: suctioning secretions if necessary
– Oxygen therapy: administration of oxygen adapted to the situation (nasal cannula, high-concentration mask (10-15L/min), or positive pressure ventilation using a bag-valve-mask)
– Preparation of intubation and mechanical ventilation equipment
– Consideration of non-invasive ventilatory support (CPAP, BiPAP) depending on severity
– Move the child to the intervention room and start continuous cardiorespiratory monitoring
-
Interventions for Altered Circulation to the Skin
An alteration in skin circulation may indicate early shock. Rapid interventions may include:
– Warming the patient if hypothermic
– Move the child to the intervention room and start continuous cardiorespiratory monitoring
General Interventions Regardless of the Altered Component
Certain interventions are essential regardless of which PAT component is altered:
– Call for help: mobilization of the pediatric resuscitation team if available
– Installation of the patient in a shock or intensive care room
– Implementation of complete multiparameter monitoring
– Calculation and preparation of emergency medication doses according to the child’s weight
– Frequent reassessment of the PAT to monitor evolution and effectiveness of interventions
– Clear and continuous communication with the care team about the child’s condition and actions taken
– Preparation for possible escalation of care (transfer to intensive care, emergency surgery, etc.)
The next step after applying the Pediatric Assessment Triangle to the patient and providing the necessary interventions is to begin the primary survey.
It is important to note that these interventions should be adapted to the child’s age, weight, and suspected pathology. Frequent reassessment of the PAT allows for rapid adjustment of care based on the evolution of the child’s condition.
The systematic application of these interventions, guided by the PAT assessment, allows for rapid and effective management of pediatric emergencies, thus optimizing the child’s chances of recovery.
