Out-of-hospital cardiac arrest (OHCA) remains one of the most formidable challenges in our practice, with generally low survival rates despite advances in cardiopulmonary resuscitation (CPR) and post-cardiac arrest care. The use of epinephrine in this context has long been a cornerstone of our protocols, but its effectiveness and impact on neurological outcomes have been questioned in recent years. The PARAMEDIC2 (Prehospital Assessment of the Role of Adrenaline: Measuring the Effectiveness of Drug Administration in Cardiac Arrest) study represents the largest and most rigorous randomized controlled trial to date on this subject. In this article, we will examine in detail the results of this crucial study, compare them to other relevant research, and discuss their implications for our daily practice.
PARAMEDIC2 Study Methodology:
The PARAMEDIC2 study is a randomized, placebo-controlled, double-blind trial conducted in the United Kingdom from December 2014 to October 2017. It included 8,014 adult patients with OHCA, divided into two groups:
-
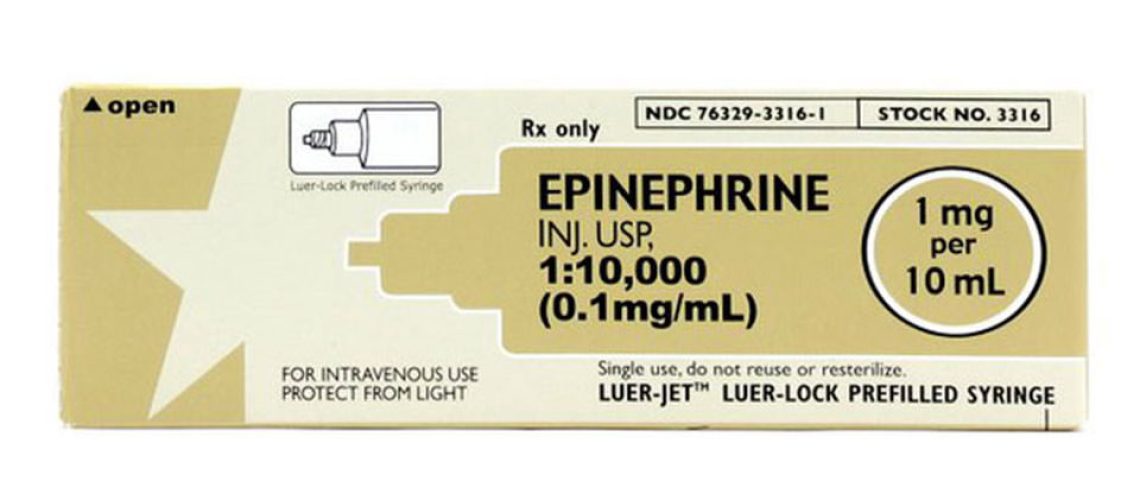
- Epinephrine group (n=4,015): administration of 1 mg of epinephrine IV or IO every 3-5 minutes.
- Placebo group (n=3,999): administration of saline solution according to the same protocol.
Exclusion criteria included pregnancy, age under 16, cardiac arrest due to anaphylaxis or asthma, and prior administration of epinephrine.
Main Results:
-
-
30-day survival:
-
– Epinephrine group: 3.2% (130/4,012 patients)
– Placebo group: 2.4% (94/3,995 patients)
– Unadjusted odds ratio: 1.39 (95% CI: 1.06-1.82, p=0.02)
– Number needed to treat (NNT) to prevent one death at 30 days: 112
-
-
Survival with favorable neurological outcome at hospital discharge (score ≤3 on the modified Rankin scale):
-
– Epinephrine group: 2.2% (87/4,007 patients)
– Placebo group: 1.9% (74/3,994 patients)
– Unadjusted odds ratio: 1.18 (95% CI: 0.86-1.61)
-
-
Return of spontaneous circulation (ROSC):
-
– Epinephrine group: 36.3%
– Placebo group: 11.7%
-
-
Transport to hospital:
-
– Epinephrine group: 50.8%
– Placebo group: 30.7%
Analysis of Results:
The PARAMEDIC2 study demonstrates that the use of epinephrine in OHCA significantly increases 30-day survival. However, this improvement in survival is not accompanied by a significant increase in favorable neurological outcomes. In fact, among survivors, a higher proportion of patients in the epinephrine group had severe neurological deficits (31.0% vs 17.8% in the placebo group).
These results raise important questions about the risk-benefit ratio of routine epinephrine use in OHCA. On one hand, epinephrine improves chances of ROSC and short-term survival. On the other hand, it seems to increase the risk of survival with significant neurological sequelae.
Comparison with Other Studies:
It is important to place the results of PARAMEDIC2 in the context of other research on the use of epinephrine in OHCA.
-
-
Lin et al. Meta-analysis (2014):
-
This meta-analysis of 14 observational studies showed that epinephrine use was associated with increased ROSC (OR 2.86, 95% CI: 2.28-3.58) and survival to admission (OR 1.53, 95% CI: 1.17-2.00), but not with improved survival to hospital discharge or favorable neurological outcomes.
-
-
PACA Study (Jacobs et al., 2011):
-
This smaller randomized controlled trial (n=534) comparing epinephrine to placebo showed no significant difference in survival to hospital discharge, but suggested a trend towards better survival with epinephrine (OR 2.2, 95% CI: 0.7-6.3).
-
-
SOS-KANTO Study (2012):
-
This Japanese observational study suggested that early administration of epinephrine (within 9 minutes of emergency call) was associated with better survival with favorable neurological outcome, while late administration was associated with poorer outcomes.
The results of PARAMEDIC2 are generally consistent with these earlier studies, showing improvement in ROSC and short-term survival, but without clear benefit on neurological outcomes.
Practical Implications:
-
-
Protocol Reevaluation:
-
The results of PARAMEDIC2 compel us to reconsider the place of epinephrine in our OHCA management protocols. Although epinephrine increases chances of ROSC and 30-day survival, the lack of improvement in favorable neurological outcomes raises important ethical questions.
-
-
Treatment Individualization:
-
These results suggest that a more nuanced and individualized approach may be necessary. For example, epinephrine use might be more beneficial in certain subgroups of patients or in specific cardiac arrest circumstances.
-
-
Importance of Early CPR and Defibrillation:
-
The study reminds us of the crucial importance of early interventions such as bystander CPR and rapid defibrillation. The NNT for epinephrine (112) is significantly higher than for these interventions (11 for early recognition of cardiac arrest, 15 for bystander CPR, and 5 for early defibrillation).
-
-
Communication with Patients and Families:
-
These results underscore the importance of clear communication with patients and their families about potential resuscitation outcomes, including the risk of survival with significant neurological deficits.
-
-
Reevaluation of Success Criteria:
-
The study prompts us to rethink our definitions of success in OHCA management. Survival alone can no longer be considered the sole criterion of success; quality of life and neurological outcomes must be taken into account.
Study Limitations and Future Research Directions:
-
-
Timing of Administration:
-
The study did not explore in detail the impact of epinephrine administration timing. Future research could focus on identifying the optimal moment for epinephrine administration.
-
-
Dosage and Administration Regimen:
-
PARAMEDIC2 used the standard dosage of 1 mg every 3-5 minutes. Future studies could explore different dosages or administration regimens.
-
-
Specific Subgroups:
-
Although the study included subgroup analysis, more in-depth research on specific populations (e.g., based on cardiac arrest etiology or initial rhythm) could be beneficial.
-
-
Brain Injury Mechanisms:
-
Additional research is needed to understand the mechanisms by which epinephrine might contribute to unfavorable neurological outcomes, particularly its impact on cerebral microcirculation.
-
-
Pharmacological Alternatives:
-
Exploration of other vasopressor agents or drug combinations could offer new perspectives for improving OHCA outcomes.
-
-
Post-Resuscitation Care:
-
The study did not standardize post-resuscitation care. Future research could examine the interaction between epinephrine use and post-cardiac arrest care strategies, such as targeted temperature management.
-
-
Long-term Quality of Life:
-
Longer-term follow-up studies, including detailed quality of life assessments, could provide valuable information on the long-term impact of epinephrine use.
Conclusion:
The PARAMEDIC2 study represents a major advance in our understanding of the role of epinephrine in OHCA management. Although it demonstrates a benefit in terms of 30-day survival, the lack of improvement in favorable neurological outcomes and the potential increase in the risk of survival with severe neurological deficits raise important questions.
As emergency physicians, we are now faced with the challenge of carefully weighing the advantages and disadvantages of epinephrine use in each situation. This study reminds us of the crucial importance of early CPR and defibrillation, while prompting us to rethink our OHCA management strategies.
As we continue to refine our protocols and seek new approaches to improve OHCA outcomes, it is essential to keep in mind that our ultimate goal is not just survival, but survival with an acceptable quality of life for our patients. The PARAMEDIC2 study pushes us to think critically about our current practices and to continue seeking ways to optimize outcomes for our cardiac arrest patients.