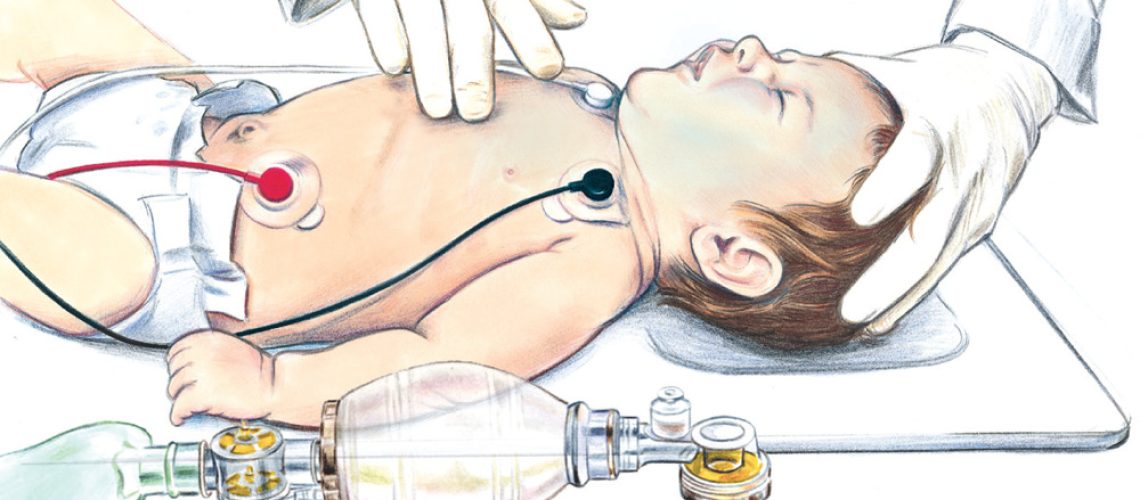
Cardiopulmonary resuscitation (CPR) is a crucial element in the management of cardiac arrests, particularly in children. A recent study published in Circulation sheds new light on the importance of chest compression pauses during in-hospital pediatric CPR. Let’s examine in detail the results of this study and their implications for clinical practice.
Study Context
Each year, more than 15,000 children suffer an in-hospital cardiac arrest in the United States, with a survival rate of less than 50%. Improving CPR techniques is therefore a major challenge to increase the chances of survival for these young patients.
The American Heart Association recommends minimizing chest compression pauses to less than 10 seconds in children. However, this recommendation was not previously supported by solid evidence in pediatrics.
The study published in Circulation aimed to fill this gap by examining the association between the duration of chest compression pauses and survival after in-hospital pediatric cardiac arrest.
Methodology
Researchers analyzed data from 562 cases of in-hospital pediatric cardiac arrests that occurred between July 2015 and December 2021, from the pediRES-Q (Quality of Pediatric Resuscitation in a Multicenter Collaborative) database.
The main criteria studied were:
– The duration of the longest chest compression pause for each event
– Survival with favorable neurological outcome (defined as a Pediatric Cerebral Performance Category score ≤3 or no change from baseline)
– Survival to hospital discharge
– Return of spontaneous circulation (ROSC)
Researchers also examined other parameters such as the presence of pauses >10 seconds or >20 seconds, the number of pauses >10 seconds and >20 seconds per 2-minute period, as well as the chest compression fraction (CCF).
Main Results
-
-
Longest Pause Duration and Survival
-
The most striking result of this study is the significant association between the duration of the longest chest compression pause and chances of survival.
For each 5-second increment in the duration of the longest pause, researchers observed:
– A 3% decrease in the relative risk of survival with favorable neurological outcome (adjusted RR: 0.97; 95% CI: 0.95-0.99; p=0.01)
– A 2% decrease in the rate of survival to hospital discharge (adjusted RR: 0.98; 95% CI: 0.96-0.99; p=0.01)
– A 7% reduction in the chances of ROSC (adjusted RR: 0.93; 95% CI: 0.91-0.94; p<0.001)
These results highlight the crucial importance of limiting the duration of chest compression pauses, particularly the longest pause, to optimize young patients’ chances of survival.
-
-
Pauses >10 seconds and >20 seconds
-
The study also examined the impact of pauses exceeding the thresholds of 10 and 20 seconds:
– The presence of a pause >10 seconds was associated with a lower probability of ROSC (adjusted RR: 0.80; 95% CI: 0.70-0.92; p=0.002)
– The presence of a pause >20 seconds was also linked to a decrease in the chances of ROSC (adjusted RR: 0.86; 95% CI: 0.77-0.96; p=0.008)
However, these associations were not statistically significant for survival to hospital discharge or survival with favorable neurological outcome.
-
-
Number of pauses >10 seconds and >20 seconds
-
The number of pauses exceeding these thresholds per 2-minute period was also studied:
– Each additional pause >10 seconds per 2-minute period was associated with a 6% reduction in the chances of ROSC (adjusted RR: 0.94; 95% CI: 0.91-0.98; p=0.001)
– Each additional pause >20 seconds per 2-minute period was linked to a 9% decrease in the probability of ROSC (adjusted RR: 0.91; 95% CI: 0.86-0.96; p<0.001)
Again, these associations were not significant for long-term survival or neurological outcome.
-
-
Chest Compression Fraction (CCF)
-
Interestingly, CCF (proportion of resuscitation time devoted to chest compressions) was not significantly associated with survival outcomes in this study. This finding contrasts with some previous studies in adults and highlights the need for a specific approach in pediatrics.
Implications for Clinical Practice
These results have important implications for pediatric CPR practice:
-
-
Priority to Limiting Long Pauses
-
The study highlights the crucial importance of limiting the duration of the longest chest compression pause. Resuscitation teams should therefore pay particular attention to this aspect, striving to keep all pauses as short as possible.
-
-
Validation of the 10-second Recommendation
-
The results support the American Heart Association’s recommendation to keep pauses below 10 seconds. Although this limit is not an absolute threshold, it seems to be a reasonable goal to optimize chances of survival.
-
-
Importance of Teamwork
-
To achieve these pause limitation objectives, effective teamwork is essential. This involves:
– Well-coordinated team choreography
– Clear and effective communication
– Thorough preparation before necessary pauses (e.g., for rhythm analysis or defibrillation)
– Use of countdowns to limit pause duration
-
-
Focus on Critical Moments
-
Special attention should be paid to moments prone to prolonged pauses, such as:
– Checking heart rhythm and pulse
– Defibrillation
– Tracheal intubation
– ECMO setup
– Bedside ultrasound
-
-
Reevaluation of CCF Importance
-
Unlike some adult studies, this study did not show a significant association between CCF and survival. This suggests that simply maximizing CCF may not be the most effective strategy in pediatrics. The emphasis should rather be on limiting prolonged pauses.
-
-
Training and Simulation
-
These results highlight the importance of integrating chest compression pause management into pediatric CPR training and simulation sessions. Teams should practice minimizing pause duration, particularly in situations prone to prolonged interruptions.
Study Limitations
Although this study provides valuable information, it’s important to recognize its limitations:
-
- Observational Nature: Being an observational study, it cannot establish a direct causal link between pause duration and survival outcomes.
-
- Limited Data on Pause Causes: The study does not provide detailed information on the specific reasons for each pause, which could have provided additional insight.
-
- Potential Underestimation of Compressions: The use of defibrillator data may have led to an underestimation of chest compressions performed before or after electrode placement.
-
- Risk of Misclassification: Although researchers checked long pauses to exclude ROSC periods, it’s possible that some shorter pauses were misclassified.
-
- Limited Statistical Power: For some secondary criteria, particularly the association between pauses >10 or >20 seconds and long-term survival, the study may lack statistical power.
-
- Potential Selection Bias: Hospitals participating in the pediRES-Q collaboration may be more committed to CPR quality than average, which could limit the generalization of results.
Future Perspectives
This study opens the way for several future research directions:
-
- Interventional Studies: Randomized controlled trials specifically targeting the reduction of long pauses could confirm the causal impact of this strategy on survival.
-
- Analysis of Pause Causes: A more in-depth study of the specific reasons for prolonged pauses could help identify targeted strategies to reduce them.
-
- Decision Support Technology: The development of real-time tools to alert teams about pause duration could be an interesting avenue to improve CPR quality.
-
- Teamwork Optimization: Research on best teamwork practices to minimize pauses could provide valuable guidance for training.
-
- Larger-scale Multicenter Studies: Studies including a larger number of centers and patients could strengthen the external validity of the results.
-
- Exploration of Differences with Adult CPR: Comparative research between pediatric and adult CPR could help better understand the specificities of each population.
Conclusion
This study provides solid evidence of the importance of limiting the duration of chest compression pauses during in-hospital pediatric CPR. It validates the American Heart Association’s recommendation to keep pauses below 10 seconds and highlights the potential impact of each additional second on chances of survival.
For practitioners, these results reinforce the need for constant attention to pause duration during CPR. They also underscore the importance of effective teamwork and thorough preparation for critical moments of resuscitation.
Although further research is needed to confirm these results and explore optimization strategies, this study provides valuable guidance for improving the quality of pediatric CPR. Ultimately, these efforts could translate into significant improvement in survival rates and neurological outcomes for young patients suffering from in-hospital cardiac arrest.
As healthcare professionals, we have a responsibility to stay informed about the latest advances in this field and integrate this knowledge into our daily practice. Every second counts during cardiac arrest, and this study reminds us of the crucial importance of maximizing the effectiveness of each of these seconds to give our young patients the best possible chance of survival.