The Pediatric Assessment Triangle (PAT)
The rapid and accurate assessment of a child’s health status in an emergency situation is a crucial skill for any healthcare professional working in a pediatric emergency department. The Pediatric Assessment Triangle (PAT) has become an essential tool in this field, offering a structured and efficient approach to quickly assess the severity of a child’s condition upon arrival at the emergency department.
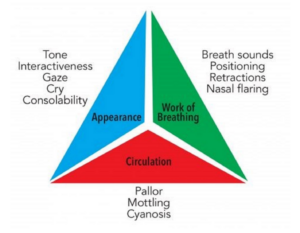
Developed by the American Academy of Pediatrics and integrated into Advanced Pediatric Life Support (APLS) and Pediatric Advanced Life Support (PALS) training, the PAT allows for a quick visual and auditory assessment, requiring no specific equipment. This method, based on observing three main components – appearance, work of breathing, and circulation to the skin – allows for rapid identification of children requiring immediate care and guides the initial steps of resuscitation.
In this article, we will explore in detail the Pediatric Assessment Triangle, its practical application, its advantages and limitations, as well as its integration into the overall management of pediatric emergencies.
Foundations of the Pediatric Assessment Triangle
Basic Principle
The PAT is based on the rapid assessment of three interdependent physiological components:
- Appearance
- Work of breathing
- Circulation
These three elements form the sides of the “triangle,” allowing for a global assessment of the child’s physiological state in just a few seconds.
Objectives of the PAT
The main objectives of the Pediatric Assessment Triangle are:
– Rapidly identify severely ill or injured children
– Establish a priority for care
– Guide the initial steps of resuscitation
– Provide a common language for communication between healthcare professionals
Components of the Pediatric Assessment Triangle
-
Appearance
Appearance is considered the most important side of the triangle, reflecting oxygenation, ventilation, cerebral perfusion, and central nervous system functioning.
Elements to evaluate:
– Tone: Is the child active, moving spontaneously, or floppy?
– Interactivity: Is the child alert, responsive to environmental stimuli?
– Consolability: Can the child be consoled or calmed?
– Gaze: Is the gaze lively and attentive or fixed and empty?
– Speech/cry: Are the cries strong and vigorous or weak and whimpering?
An altered appearance may indicate severe neurological, respiratory, circulatory, or metabolic impairment.
-
Work of breathing
Assessing the work of breathing allows for quick identification of respiratory distress or impending respiratory failure.
Elements to evaluate:
– Abnormal position: Sitting position, tripod position, refusal to lie down
– Retractions: Supraclavicular, intercostal, subcostal
– Nasal flaring
– Audible breathing sounds: Stridor, wheezing, grunting
– Tachypnea or bradypnea
Increased work of breathing usually indicates respiratory pathology but can also be observed in other situations such as metabolic acidosis.
-
Circulation to the skin
Assessing circulation to the skin allows for a quick appreciation of peripheral tissue perfusion.
Elements to evaluate:
– Color: Pallor, cyanosis, mottling
– Capillary refill time (CRT): Normally < 2 seconds
An alteration in skin circulation may indicate shock, severe dehydration, or circulatory insufficiency of another origin.
Interpretation of the Pediatric Assessment Triangle
The interpretation of the PAT is done by analyzing the different possible combinations of alterations in the three components. Generally, seven physiological states are distinguished:
**Stable**: No altered components
**Respiratory distress**: Altered work of breathing, normal appearance and circulation
**Respiratory failure**: Altered work of breathing and appearance, normal circulation
**Compensated shock**: Altered circulation, normal appearance and work of breathing
**Decompensated shock**: Altered circulation and appearance, normal or altered work of breathing
**Central nervous system dysfunction**: Altered appearance, normal work of breathing and circulation
**Cardiopulmonary failure**: All three components are altered
This categorization allows for quickly orienting initial management and anticipating needs in terms of resources and interventions.
Practical Application of PAT in Pediatric Emergencies
Integration into triage
The PAT is particularly useful during initial patient triage. It allows for a rapid and standardized assessment, facilitating the prioritization of care. Its use in conjunction with usual triage scales (such as the Canadian Triage and Acuity Scale) allows for refining the assessment of urgency.
Continuous reassessment
The PAT is not limited to initial assessment. It should be repeated regularly to monitor the evolution of the child’s condition and the effectiveness of interventions put in place.
Advantages of the Pediatric Assessment Triangle
Speed and simplicity
The PAT can be performed in a few seconds, without requiring specific equipment. This speed is crucial in emergency situations where every second counts.
Standardization of assessment
By providing a structured framework for initial assessment, the PAT reduces inter-observer variability and improves consistency in care.
Effective communication
The PAT offers a common language for different caregivers, facilitating communication within the care team and during handovers.
Adaptability
Although developed for pediatric emergencies, the principle of the PAT can be applied in other contexts, such as pre-hospital medicine or adult emergencies.
Limitations and Considerations
Limited specificity
The PAT is a rapid screening tool and not a diagnostic tool. It does not replace a complete clinical assessment and complementary examinations when necessary.
Physiological variability
Normal parameters vary according to the child’s age. A good knowledge of pediatric physiology is necessary for correct interpretation of the PAT.
Masked pathologies
Some pathologies may not be immediately detectable by the PAT, particularly in their early stages.
Training required
Although simple in appearance, optimal use of the PAT requires training and regular practice.
Integration of PAT into Overall Management
The Pediatric Assessment Triangle should not be considered as an isolated tool, but as the first step in a systematic approach to the child in emergency. It naturally integrates into the sequence:
PAT → Primary assessment (ABCDE) → Immediate vital interventions → Targeted history → Complete physical examination → Secondary and tertiary assessments
This approach allows for structured management, ranging from rapid initial assessment to more in-depth and specific management.
Training and Implementation
For effective use of the PAT in a pediatric emergency department, several steps are recommended:
**Initial training**: All team members should be trained in the use of the PAT, ideally as part of broader training such as APLS or PALS.
**Simulation exercises**: Regular simulation sessions allow practicing the use of the PAT in different clinical scenarios.
**Standardized protocols**: Integration of the PAT into triage and initial management protocols ensures systematic use.
**Audit and feedback**: Regular evaluations of the use of the PAT and its impact on patient management help identify areas for improvement.
**Continuous training**: Regular reminders and updates on the use of the PAT maintain team skills.
Conclusion
The Pediatric Assessment Triangle is a powerful and effective tool for rapid assessment of children in emergency situations. Its ease of use, combined with its ability to quickly provide crucial information about the child’s physiological state, makes it an essential element in the toolkit of any practitioner working in a pediatric emergency department.
Although the PAT does not replace a complete clinical assessment, it offers a structured framework to quickly initiate appropriate care and prioritize interventions. Its systematic use, combined with adequate training and integration into standardized care protocols, can significantly improve the quality and safety of care provided to children in emergency situations.
In an environment where speed and accuracy are crucial, the Pediatric Assessment Triangle stands as a valuable ally for healthcare professionals, contributing to saving lives and improving outcomes for young patients.
References
- Dieckmann RA, Brownstein D, Gausche-Hill M. The pediatric assessment triangle: a novel approach for the rapid evaluation of children. Pediatr Emerg Care. 2010;26(4):312-315.
- American Academy of Pediatrics, American College of Emergency Physicians. APLS: The Pediatric Emergency Medicine Resource, 5th ed. Jones & Bartlett Learning, 2011.
- Horeczko T, Enriquez B, McGrath NE, Gausche-Hill M, Lewis RJ. The Pediatric Assessment Triangle: accuracy of its application by nurses in the triage of children. J Emerg Nurs. 2013;39(2):182-189.
- ishbi AEF, Reeves PT. Pediatric Assessment. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024.
- American Heart Association. Pediatric Advanced Life Support Provider Manual. American Heart Association, 2020.