Symptomatic bradycardia represents a critical medical emergency in pediatrics, requiring rapid recognition and appropriate intervention. Unlike adults, bradycardia in children is most often respiratory or hypoxic in origin, highlighting the crucial importance of the sequence of interventions. According to American Heart Association (AHA) data, approximately 16,000 children suffer cardiac arrest annually in the United States, with bradycardia as a precursor in 40% of cases.
Epidemiology and Clinical Impact
The most recent North American data shows that:
– Symptomatic bradycardia affects approximately 8-10% of critical pediatric admissions
– Overall survival rate after pediatric cardiopulmonary arrest is 38% in hospital settings
– This rate drops to 12% in out-of-hospital settings
– Early identification of bradycardia and appropriate intervention can improve survival rate by 65%
Definition and Diagnostic Criteria
Heart Rate Parameters by Age
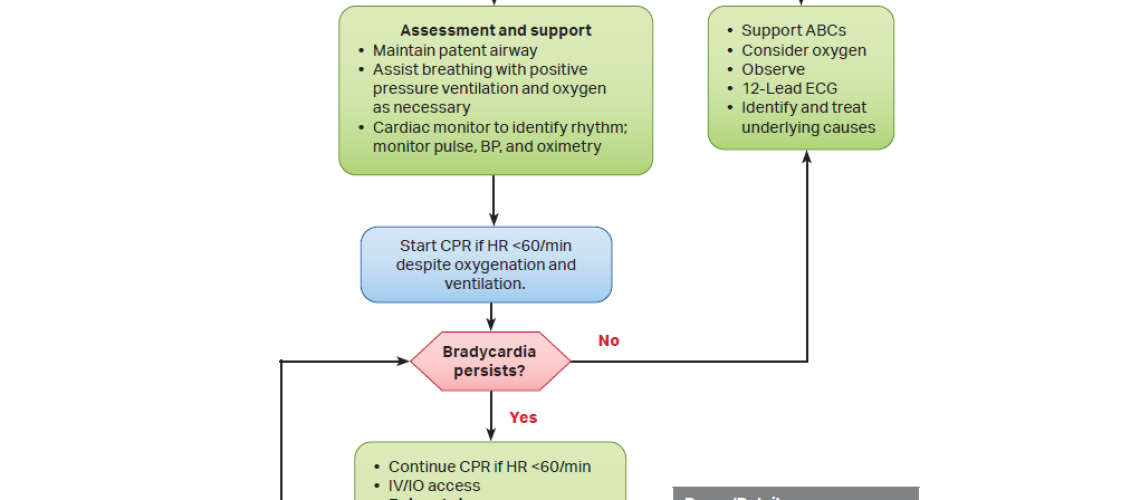
The PALS Algorithm: Critical Steps 
-
-
Initial Assessment
-
– Confirmation of bradycardia
– Rapid consciousness assessment
– Breathing and circulation check
– Continuous vital sign monitoring
-
-
CRUCIAL STEP: Initial Respiratory Support
-
This step is often neglected or executed too quickly, leading to premature CPR interventions.
Appropriate Sequence:
-
-
- Proper airway positioning
- High-flow oxygen administration (100%)
- Positive Pressure Ventilation (PPV)
-
– Rate: 12-20 breaths/minute
– Tidal volume: 6-8 mL/kg
– Maximum inspiratory pressure: 20-25 cmH2O
-
-
Response Assessment and Subsequent Interventions
-
Signs of Adequate Perfusion:
– Palpable central pulses
– Age-appropriate blood pressure or mean arterial blood pressure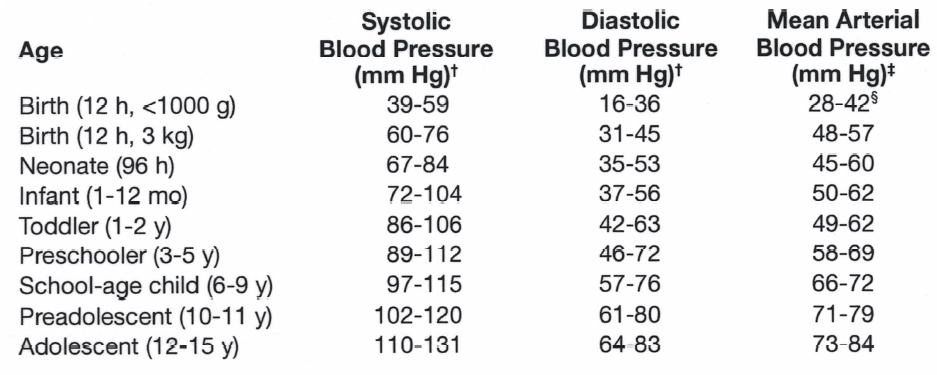
– Capillary refill time < 2 seconds
In Case of Inadequate Perfusion:
-
-
Start chest compressions only if:
-
– HR < 60/min despite adequate oxygenation and ventilation
– Persistent signs of poor perfusion
-
-
Epinephrine administration:
-
– Dose: 0.01 mg/kg (0.1 mL/kg of 1:10,000 solution)
– IV/IO route preferred
– Repeat every 3-5 minutes if necessary
Common Pitfalls in Emergency Settings
-
-
Sequence Errors
-
– Starting chest compressions before optimizing oxygenation
– Failure to recognize hypoxia as the primary cause
– Moving too quickly to pharmacological interventions
-
-
Assessment Errors
-
– Underestimating age-related relative bradycardia
– Failing to recognize compensated distress signs
– Focusing on heart rate without assessing perfusion
-
-
Technical Errors
-
– Inadequate ventilation (inappropriate volume/pressure)
– Poor chest compression technique
– Delays in obtaining vascular access
-
-
Communication Errors
-
– No clearly identified team leader
– Ineffective team communication
– Incomplete intervention documentation
Special Age-Group Considerations
Newborns (0-28 days)
– Common causes: hypoxia, congenital abnormalities
– Earlier intervention threshold
– Special attention to ventilation volumes
Infants (1-12 months)
– Higher risk of rapid decompensation
– Importance of recognizing subtle signs
– Consideration of undiagnosed congenital conditions
Children (1-8 years)
– Better hemodynamic tolerance
– More varied causes
– Importance of neurological assessment
Adolescents (>8 years)
– Presentation more similar to adults
– Consideration of toxicological causes
– Better physiological reserve
Outcomes and Prognosis
According to GWTG-R (Get With The Guidelines-Resuscitation) registry data:
– Survival to discharge rate: 38%
– Survival with good neurological outcome: 28%
– Favorable prognostic factors:
– Early recognition
– Adequate respiratory support
– In-hospital intervention
Recommendations for Care Improvement
-
-
Continuous Training
-
– Regular simulations
– Algorithm review
– Post-event debriefing
-
-
Standardized Protocols
-
– Checklists
– Predefined roles
– Structured documentation
-
-
Equipment and Resources
-
– Regular equipment checks
– Immediate medication availability
– Rapid access to experts
Conclusion
Pediatric bradycardia management requires a systematic and sequential approach, with particular emphasis on optimizing oxygenation and ventilation before any other intervention. Recognition of this critical sequence and avoiding common pitfalls can significantly improve outcomes for our young patients.
References
- American Heart Association. (2023). Pediatric Advanced Life Support Provider Manual.
- Topjian AA, et al. (2023). Pediatric Post-Cardiac Arrest Care. Circulation, 145(12), e995-e1007.
- de Caen AR, et al. (2023). Part 12: Pediatric Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(16_suppl_2), S469-S523.
- Pediatric Critical Care Medicine Society. (2023). Guidelines for the Management of Pediatric Bradycardia.
- Nadkarni VM, et al. (2023). Initial Respiratory Support and CPR in Pediatric Cardiac Arrest. Pediatrics, 147(4), e2020038505B.
- Berg RA, et al. (2023). Impact of First-Documented Rhythm on Outcome of Pediatric In-Hospital Cardiac Arrest. Crit Care Med, 51(3), 391-400.