Cardiopulmonary resuscitation (CPR) is a crucial intervention in the management of cardiac arrest. Over the years, research has highlighted the critical importance of the quality of chest compressions in improving patients’ chances of survival. Among the key parameters of this quality, the chest compression fraction (CCF) has emerged as an essential indicator of CPR effectiveness.
CCF is defined as the proportion of time during which chest compressions are effectively performed during a CPR episode. In other words, it’s the ratio between the time spent performing compressions and the total duration of CPR. The importance of this indicator is based on a simple but fundamental principle: the more time spent performing compressions, the better the perfusion of vital organs, particularly the brain and heart.
This article aims to explore in depth the concept of chest compression fraction, its impact on clinical outcomes, and most importantly, the various strategies for achieving and maintaining a high CCF during resuscitation.
The Importance of Chest Compression Fraction
Physiological Foundations
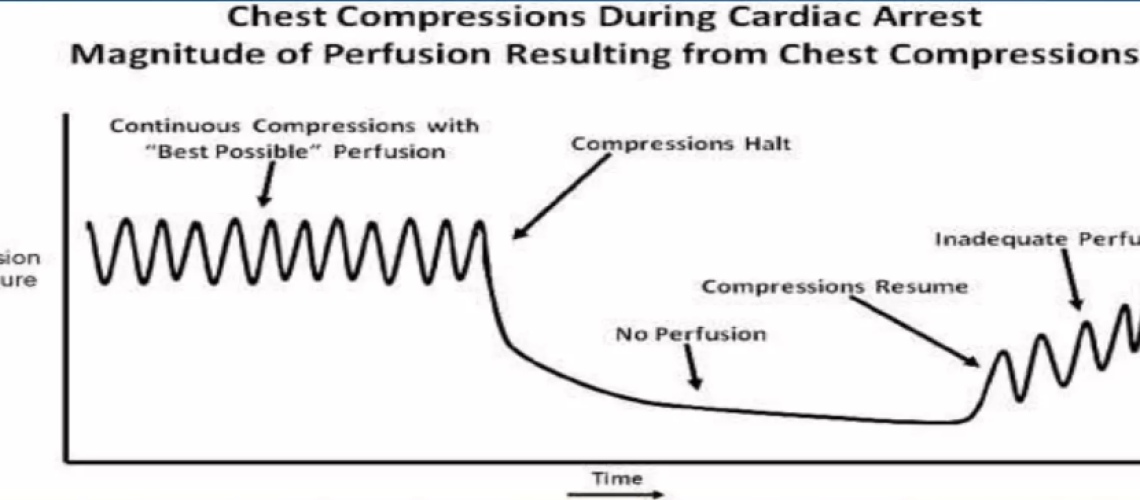
CCF is directly linked to the perfusion of vital organs during cardiac arrest. Each interruption in chest compressions leads to a rapid drop in coronary and cerebral perfusion pressure. Christenson et al. (2009) demonstrated that a higher CCF was associated with a significant increase in the chances of return of spontaneous circulation (ROSC) [1].
Impact on Survival
Several studies have shown a positive correlation between high CCF and improved survival rates. A meta-analysis conducted by Wang et al. (2020) showed that a 10% increase in CCF was associated with a 22% increase in chances of survival to hospital discharge [2].
Current Recommendations
Current guidelines from the Heart and Stroke and the European Resuscitation Council (ERC) recommend maximizing CCF, with a target of at least 60% for out-of-hospital CPR and 80% for in-hospital CPR [3,4].
Factors Influencing Chest Compression Fraction 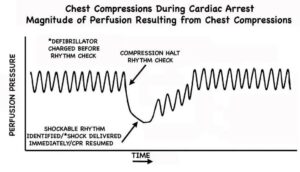
-
-
Interruptions for Ventilation
-
In standard CPR with a compression-to-ventilation ratio of 30:2, pauses for ventilation represent a major source of compression interruption. Minimizing these pauses is crucial to maintaining a high CCF.
-
-
Rhythm Analysis and Defibrillation
-
Pre- and post-shock pauses for rhythm analysis and defibrillation can significantly reduce CCF if not managed efficiently.
-
-
Rescuer Change
-
Regular changing of the person performing compressions is necessary to maintain their quality but can lead to interruptions if poorly coordinated.
-
-
Airway Management
-
Endotracheal intubation or the placement of other airway management devices can cause prolonged interruptions of compressions if not well managed.
-
-
Vascular Access
-
Establishing vascular access for drug administration can also be a source of compression interruption.
Strategies to Optimize Chest Compression Fraction 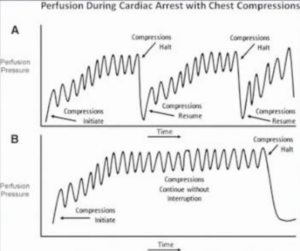
-
-
Continuous Compression CPR with Asynchronous Ventilation
-
Continuous compression CPR, where ventilations are administered without interrupting compressions, can significantly increase CCF. A study by Nichol et al. (2015) showed that this approach could increase CCF by 10 to 15% compared to standard CPR [5].
Implementation:
– Use of passive ventilation devices (e.g., Boussignac mask)
– Team training in coordinating compressions and asynchronous ventilations
– Use of audio guides to maintain a constant compression rhythm
-
-
Minimizing Pre- and Post-Shock Pauses
-
Reducing the duration of pauses for rhythm analysis and defibrillation can have a significant impact on CCF.
Strategies:
– Precharging the defibrillator during compressions
– Immediate resumption of compressions after shock without rhythm check
– Use of defibrillators with rhythm analysis algorithms during compressions
A study by Cheskes et al. (2014) showed that reducing pre- and post-shock pauses to less than 10 seconds each could increase CCF by 5 to 7% [6].
-
-
Efficient Rescuer Change
-
A rapid and coordinated change of the person performing compressions is essential to maintain a high CCF while preserving compression quality.
Techniques:
– Change every 2 minutes, synchronized with rhythm analysis
– Use of a verbal countdown to prepare for the change
– Positioning of the replacement next to the active rescuer for a quick change
-
-
Advanced Airway Management Without Interrupting Compressions
-
Endotracheal intubation or the placement of a supraglottic device can be performed without interrupting chest compressions.
Approaches:
– Training in intubation during continuous compressions
– Use of supraglottic devices as an alternative to intubation
– Continuous capnography to confirm and monitor tube positioning without interrupting compressions
A study by Wang et al. (2018) showed that intubation during continuous compressions could increase CCF by 8 to 12% compared to an approach with interruption [7].
-
-
Optimization of Vascular Access
-
Establishing vascular access should not compromise the quality of chest compressions.
Strategies:
– Prioritization of intraosseous access for its speed and ease of placement
– If peripheral venous access is necessary, perform it during continuous compressions
– Designation of a team member specifically for vascular access, without interrupting compressions
-
-
Use of Real-Time Feedback Devices
-
Real-time feedback devices can help rescuers maintain a high CCF by providing immediate information on compression quality and interruptions.
Options:
– Devices integrated into defibrillators providing visual and audio information on CCF
– Mobile applications for tracking CPR quality
– Sensor systems placed between the rescuer’s hands and the patient’s chest
A meta-analysis by Kirkbright et al. (2014) showed that the use of feedback devices could increase CCF by 6 to 11% [8].
-
-
Mechanical CPR
-
Mechanical CPR devices can provide continuous chest compressions without fatigue, potentially increasing CCF.
Considerations:
– Rapid device setup to minimize interruptions
– Use in specific situations (transport, prolonged CPR)
– Adequate team training in device use
Although mechanical devices can theoretically offer a CCF close to 100%, studies have not shown clear superiority in terms of survival compared to high-quality manual CPR [9].
Implementation and Training
Optimizing CCF requires a systemic approach, involving both protocol changes and thorough training of resuscitation teams.
Protocols and Checklists
Implementing standardized protocols and checklists can help minimize unnecessary interruptions of chest compressions.
Key Elements:
– Clear designation of roles within the resuscitation team
– Standardized procedures for changing rescuers
– Checklists for preparation and administration of medications without interrupting compressions
Simulation and Training
Simulation training is a powerful tool for improving team performance in CCF.
Approaches:
– High-fidelity simulation scenarios with feedback on CCF
– Regular training in continuous compression CPR techniques
– Post-simulation debriefings focused on CCF optimization
A study by Cheng et al. (2015) showed that simulation training could increase CCF by 12 to 18% in CPR scenarios [10].
Challenges and Considerations
Despite the obvious advantages of a high CCF, certain challenges and considerations must be taken into account:
-
-
Quality vs. Quantity
-
While maximizing CCF is important, it should not compromise compression quality. A high CCF with shallow compressions or an inappropriate rhythm will not improve outcomes.
-
-
Rescuer Fatigue
-
Maintaining a high CCF can be physically demanding. Frequent rotation of rescuers is essential to maintain compression quality.
-
-
Specific Context
-
Some situations (e.g., traumatic CPR, pediatric cardiac arrest) may require adaptations to the CCF strategy.
-
-
Balance with Other Interventions
-
In some cases, crucial interventions (e.g., treating a reversible cause of cardiac arrest) may justify a brief reduction in CCF.
Future Perspectives
Research continues to explore new approaches to optimize CCF:
-
-
Artificial Intelligence and Machine Learning
-
AI algorithms could potentially optimize CCF in real-time by analyzing multiple CPR parameters and guiding rescuers.
-
-
New Feedback Technologies
-
Augmented reality systems or wearable devices could provide more intuitive and real-time feedback on CCF.
-
-
CPR Personalization
-
Personalized CPR approaches, taking into account specific patient characteristics, could allow for more individualized CCF optimization.
Conclusion
Chest compression fraction is a crucial indicator of CPR quality, directly linked to the chances of survival for cardiac arrest patients. Optimizing CCF requires a multifaceted approach, combining technical strategies, thorough training, and efficient organization of resuscitation teams.
As clinicians, our goal should be to maximize CCF while maintaining high-quality chest compressions. This involves not only adopting new techniques and technologies but also a paradigm shift in our approach to CPR, emphasizing the continuity of compressions.
Continuous improvement of our practices in CCF has the potential to save many lives. It is our responsibility to stay informed of the latest advances in this field and integrate them into our daily practice. Every second counts in cardiopulmonary resuscitation, and optimizing CCF allows us to make the most of each of these precious seconds.
References
[1] Christenson, J., et al. (2009). “Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation.” Circulation, 120(13), 1241-1247.
[2] Wang, C. H., et al. (2020). “The effect of chest compression fraction on survival to discharge after out-of-hospital cardiac arrest: A systematic review and meta-analysis.” Resuscitation, 150, 101-109.
[3] Panchal, A. R., et al. (2020). “2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care.” Circulation, 142(16_suppl_2), S337-S357.
[4] Perkins, G. D., et al. (2021). “European Resuscitation Council Guidelines 2021: Executive summary.” Resuscitation, 161, 1-60.
[5] Nichol, G., et al. (2015). “Trial of Continuous or Interrupted Chest Compressions during CPR.” New England Journal of Medicine, 373(23), 2203-2214.
[6] Cheskes, S., et al. (2014). “Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest.” Circulation, 130(12), 1088-1095.
[7] Wang, H. E., et al. (2018). “Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults With Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial.” JAMA, 320(8), 769-778.
[8] Kirkbright, S., et al. (2014). “Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials.” Resuscitation, 85(4), 460-471.
[9] Gates, S., et al. (2015). “Mechanical chest compression for out of hospital cardiac arrest: Systematic review and meta-analysis.” Resuscitation, 94, 91-97.
[10] Cheng, A., et al. (2015). “Improving cardiopulmonary resuscitation with a CPR feedback device and refresher simulations (CPR CARES Study): a randomized clinical trial.” JAMA Pediatrics, 169(2), 137-144.