Cardiac arrest remains one of the leading causes of mortality worldwide, with over 40,000 out-of-hospital cardiac arrests (OHCA) occurring each year in Canada. In response to this reality, Heart and Stroke has developed and continues to refine the Advanced Cardiovascular Life Support (ACLS) algorithm for adult cardiac arrest. This algorithm has become the cornerstone of cardiac arrest management in emergency departments worldwide.
In this article, we will explore in depth the current ACLS algorithm, focusing on Heart and Stroke recommendations. We will address the specific challenges encountered by emergency physicians during its application and examine new developments in this crucial area of emergency medicine.
Current ACLS Algorithm for Adult Cardiac Arrest
Overview
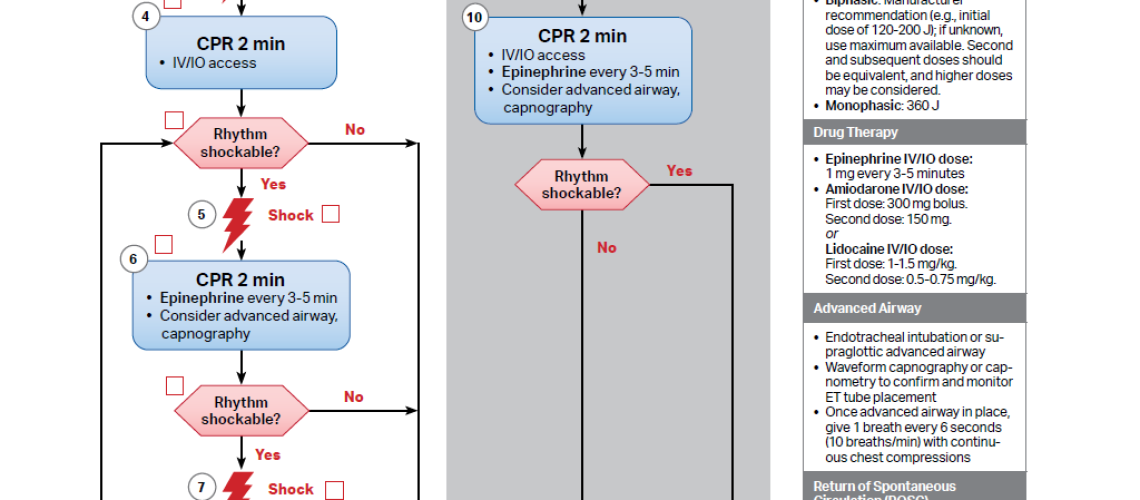
The ACLS algorithm for adult cardiac arrest is designed to provide a systematic, evidence-based approach to cardiac arrest management. It emphasizes rapid arrest recognition, immediate initiation of high-quality CPR, and identification and treatment of shockable and non-shockable rhythms.
Key Algorithm Steps
-
-
**Recognition of cardiac arrest and emergency system activation**

-
– Check for unresponsiveness and absence of normal breathing
– Activate in-hospital emergency system or call 911 if outside the hospital
-
-
**Begin high-quality CPR**
-
– Chest compressions at a rate of 100-120/min
– Compression depth of 5-6 cm (2-2.4 inches)
– Allow complete chest recoil
– Minimize compression interruptions
– Avoid excessive ventilation
-
-
**Early defibrillation**
-
– Attach defibrillator/monitor as soon as available
– Use paddle mode or self-adhesive electrodes
– Interrupt compressions only for rhythm analysis and defibrillation
-
-
**Rhythm assessment and appropriate actions**
-
– Shockable rhythms (VF/pulseless VT): immediate defibrillation
– Non-shockable rhythms (asystole/PEA): continue CPR and administer epinephrine
-
-
**Advanced airway management**
-
– Consider endotracheal intubation or supraglottic device
– Use capnography to confirm and monitor tube placement
-
-
**Vascular access**
-
– Establish IV/IO access for medication administration
-
-
**Medication administration**
-
– Epinephrine: 1 mg IV/IO every 3-5 minutes
-
-
-
- For PEA/Asystole: administer as early as possible
- For VF/pulseless VT: administer only when refractory to shock
-
-
– Amiodarone (300mg, 150mg) or Lidocaine (1.5mg/kg, 0.75mg/kg) for refractory VF/VT
-
-
**Treat reversible causes**
-
– Identify and treat the 5Hs and 5Ts
Hypoxia Toxins
Hypovolemia Tamponade
Hypo/hyperkalemia Tension pneumothorax
H+ (Acidosis) Thrombosis (coronary)
Hypothermia Thrombosis (pulmonary)
Importance of High-Quality CPR
High-quality CPR remains the cornerstone of successful resuscitation. The 2020 Heart and Stroke guidelines continue to emphasize the importance of high-quality chest compressions [1]. A study published in Resuscitation in 2019 showed that improving CPR quality was associated with a significant increase in survival to hospital discharge (OR 1.31, 95% CI 1.17-1.47) [2].
Specific Challenges for Emergency Physicians
-
-
Time and Resource Management
-
Emergency physicians often must manage multiple critical patients simultaneously. In the case of cardiac arrest, rapidly coordinating a resuscitation team while continuing to supervise other patients can be a major challenge.
**Strategies:**
– Implementation of rapid alert systems to quickly mobilize the resuscitation team
– Use of standardized checklists and protocols to ensure consistent response
– Regular training in crisis management and teamwork
-
-
Minimizing CPR Interruptions
-
CPR interruptions, even brief ones, can have a significant impact on outcomes. A study published in Circulation in 2020 showed that each 10% increase in CPR fraction (time spent performing chest compressions) was associated with a 13% increase in odds of survival to hospital discharge (OR 1.13, 95% CI 1.09-1.18) [3]. During resuscitation, the team should achieve at least 80% compression fraction and aim for 90%.
**Strategies:**
– Use of real-time CPR feedback devices
– Create a CPR coach position within the resuscitation team
– Implementation of “charging during compressions” technique to minimize pre-shock pauses
– 15-second countdown before rhythm check to take pulse and prepare for compressor change
– Training in CPR with minimal provider changes
-
-
Advanced Airway Management
-
The choice and timing of advanced airway management remain controversial. A meta-analysis published in JAMA in 2019 showed that endotracheal intubation during cardiac arrest was not associated with better survival compared to bag-mask ventilation (RR 1.00, 95% CI 0.84-1.20) [4].
**Strategies:**
– Prioritization of CPR and early defibrillation over immediate intubation
– Use of supraglottic devices as alternatives to endotracheal intubation (Laryngeal mask or IGel)
– Systematic incorporation of capnography to confirm and monitor tube placement
-
-
Identification and Treatment of Reversible Causes
-
Emergency physicians must rapidly identify and treat potentially reversible causes of cardiac arrest (the 5Hs and 5Ts) while continuing resuscitation efforts.
**Strategies:**
– Use of cognitive aids for the 5Hs and 5Ts
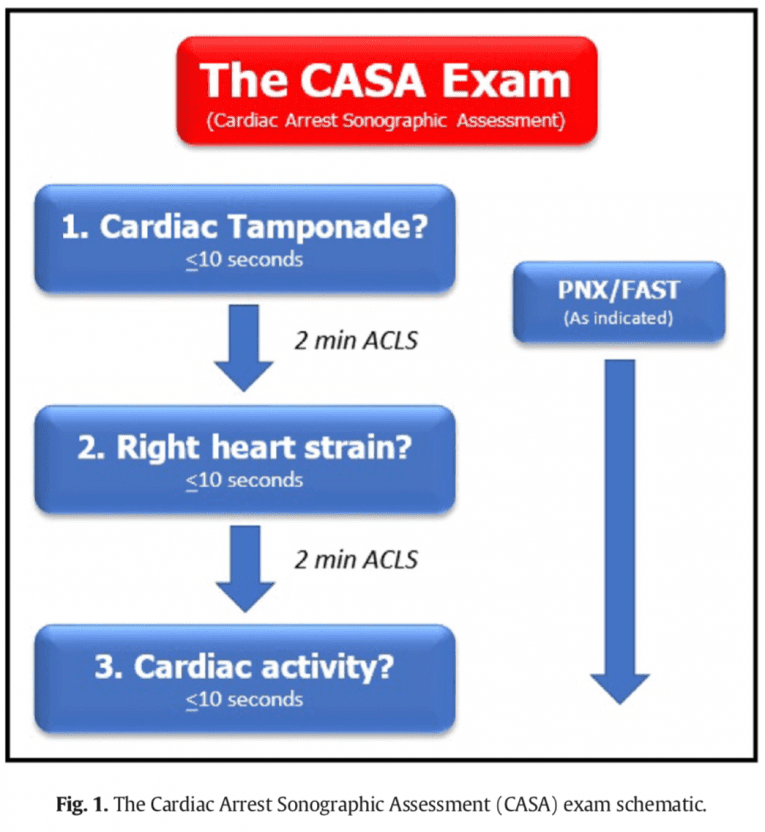
– Integration of point-of-care ultrasound (POCUS) into the resuscitation algorithm (CASA Protocol) The CASA Protocol: Optimizing Ultrasound in Cardiac Arrest without Compromising CPR – COM-BOS
– Regular training on cardiac arrest scenarios with reversible causes
-
-
Decision-Making Regarding Termination of Efforts
-
The decision to terminate resuscitation efforts is one of the most difficult faced by emergency physicians. A study published in the New England Journal of Medicine in 2019 showed that the median duration of resuscitation for patients who survived to hospital discharge was 20 minutes, compared to 32 minutes for those who did not survive [5].
**Strategies:**
– Development of institutional protocols to guide termination decisions
– Use of validated prognostic scores such as the OHCA (Out-of-Hospital Cardiac Arrest) score
– Training in family communication in end-of-life situations
New Developments and Technologies
-
-
Mechanical Chest Compression Devices
-
Mechanical chest compression devices, such as LUCAS and AutoPulse, have been developed to provide consistent, high-quality chest compressions. However, a 2019 Cochrane meta-analysis found no clear evidence of survival benefit compared to manual CPR (RR 0.95, 95% CI 0.85-1.07) [6]. Nevertheless, these devices can be useful in certain situations, such as during patient transport or during prolonged procedures, or in emergency departments with minimal staff.
-
-
Extracorporeal Membrane Oxygenation (ECMO)
-
ECMO is increasingly being used as rescue therapy in cases of refractory cardiac arrest. A cohort study published in The Lancet in 2020 showed that ECMO was associated with improved survival with good neurological outcome in selected patients with refractory cardiac arrest (OR 1.96, 95% CI 1.18-3.27) [7].
-
-
Point-of-Care Ultrasound (POCUS) Use
-
The integration of POCUS into the ACLS algorithm is gaining popularity. A meta-analysis published in Resuscitation in 2019 showed that POCUS use during resuscitation was associated with improved short-term survival (OR 2.83, 95% CI 1.78-4.49) [8]. POCUS can help identify reversible causes of cardiac arrest and guide interventions.
-
-
Real-Time CPR Feedback Systems
-
Real-time feedback systems, such as the CPRmeter or ZOLL R Series, provide instant information on CPR quality. A randomized study published in Circulation in 2021 showed that the use of these devices was associated with significant improvement in CPR quality and a trend toward better survival (OR 1.22, 95% CI 0.98-1.52) [9].
Conclusion
The ACLS algorithm for adult cardiac arrest remains an essential tool for emergency physicians in managing one of the most critical situations in emergency medicine. While the algorithm provides a structured framework, its effective application requires deep understanding, regular practice, and adaptation to specific challenges encountered in the emergency department environment.
Emergency physicians must stay current with the latest recommendations and new developments in this constantly evolving field. Judicious integration of new technologies, while maintaining focus on the fundamental principles of high-quality CPR and early defibrillation, offers the best chance of improving outcomes for cardiac arrest patients.
Continuous training, regular simulations, and post-event analysis are essential for maintaining and improving resuscitation skills. Ultimately, the ability to effectively apply the ACLS algorithm, overcome specific challenges, and integrate new advances can make the difference between life and death for our patients.
References
[1] Panchal AR, et al. 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(16_suppl_2):S337-S357.
[2] Sutton RM, et al. Association Between Chest Compression Rates and Clinical Outcomes Following In-Hospital Cardiac Arrest at a Tertiary Children’s Hospital. Resuscitation. 2019;139:208-216.
[3] Vellano K, et al. The Association of Chest Compression Release Velocity and Survival With Favorable Neurologic Outcome After Out-of-Hospital Cardiac Arrest. Circulation. 2020;142(Suppl_4):A152.
[4] Granfeldt A, et al. Advanced Airway Management During Adult Cardiac Arrest: A Systematic Review. JAMA. 2019;321(1):57-67.
[5] Reynolds JC, et al. Association Between Duration of Resuscitation and Favorable Outcome After Out-of-Hospital Cardiac Arrest: Implications for Prolonging or Terminating Resuscitation. Circulation. 2019;139(25):2701-2709.
[6] Wang PL, Brooks SC. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2019;3:CD007260.
[7] Yannopoulos D, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396(10265):1807-1816.
[8] Tsou PY, et al. Accuracy of point-of-care focused echocardiography in predicting outcome of resuscitation in cardiac arrest patients: A systematic review and meta-analysis. Resuscitation. 2019;137:75-83.
[9] Hostler D, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2021;372:m4704.